Huntington’s Disease Gene Therapy Breakthrough: What You Need to Know
Introduction
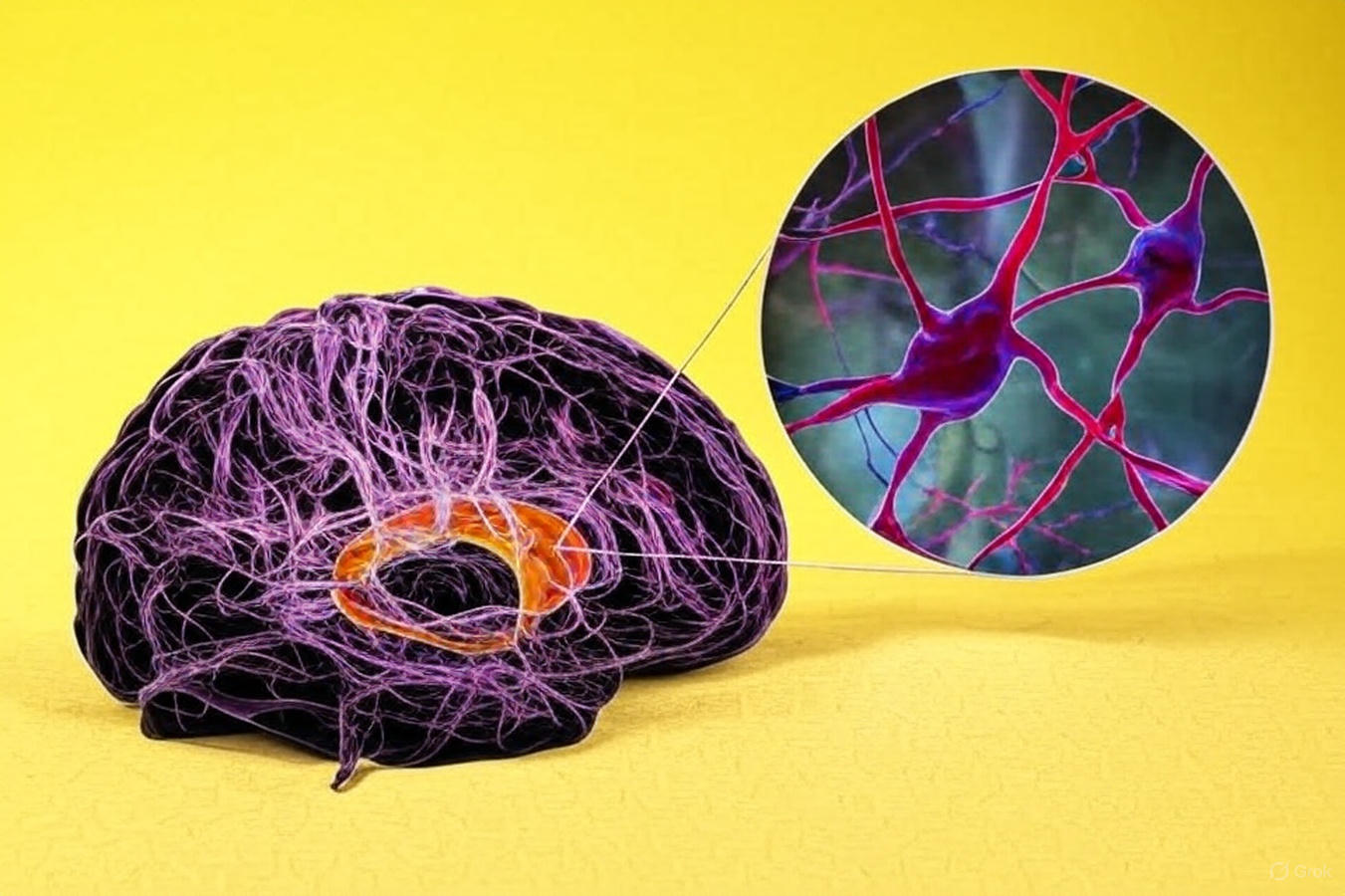
Huntington’s disease, a devastating hereditary neurological disorder, has been successfully treated for the first time through gene therapy. Announced by @Dexerto on September 24, 2025, this milestone offers hope to thousands of families worldwide. The post featured an MRI brain scan and a DNA illustration, highlighting the scientific innovation behind this breakthrough.
Huntington’s disease has been treated successfully for the first time in a gene therapy trial pic.twitter.com/UIyRaTIYaq
— Dexerto (@Dexerto) September 24, 2025
What is Huntington’s Disease?
Huntington’s disease is caused by a mutation in the huntingtin gene, producing a toxic protein that damages brain neurons. Symptoms include:
- Involuntary movements (chorea)
- Cognitive decline
- Psychiatric issues such as depression and irritability
Typically appearing between ages 30 and 50, Huntington’s is autosomal dominant, meaning there’s a 50% chance of inheritance. Without treatment, patients often face 10–20 years of progressive decline.
The Gene Therapy Breakthrough
The pioneering therapy, AMT-130, uses a one-time brain infusion to silence the defective huntingtin gene. Key points include:
- Developed by uniQure and tested in Phase I/II trials
- Slowed disease progression by up to 75% over three years
- Delivered directly into the brain to protect neurons and reduce toxic protein levels
The MRI image shared illustrates affected brain regions, such as the basal ganglia and cerebral cortex, while the DNA illustration symbolizes the gene-editing mechanism.
Implications and Future Prospects
The therapy could submit for FDA approval in early 2026, potentially offering:
- Extended independence and improved life quality
- Early intervention possibilities for at-risk individuals
- A blueprint for treating other genetic disorders
The breakthrough demonstrates how modern science can target root causes at the molecular level, not just manage symptoms.
Challenges Ahead
Despite its promise, challenges remain:
- Complex surgical procedure may limit access
- High cost could impact availability
- Long-term safety and durability still under evaluation
Public discourse on platforms like X reflects both hope and cautious skepticism, particularly regarding equitable access to such advanced therapies.
FAQs
Q1: Can Huntington’s disease be cured permanently?
Currently, there is no permanent cure, but gene therapy significantly slows progression and may prevent symptom onset in future patients.
Q2: How is gene therapy administered for Huntington’s?
Through a one-time infusion directly into the brain, targeting the defective gene and reducing toxic protein production.
Q3: Who can access this therapy?
Initially, trial participants and later patients approved by regulatory agencies; widespread access will depend on approval and healthcare policies.
Q4: Are there side effects?
Short-term side effects can include surgical risks and inflammation. Long-term data is being collected.
Q5: Could this therapy help other genetic disorders?
Yes, the same principles may be applied to other neurodegenerative or inherited diseases in the future.
Conclusion
The @Dexerto post marks a historic moment in neurology and genetic medicine. Huntington’s disease, once seen as inevitable and untreatable, now shows hope of being manageable. While challenges in accessibility, cost, and long-term safety remain, this breakthrough provides a glimpse of a future where genetic disorders may no longer dictate life’s course.
This achievement is not just a medical milestone but an intellectual triumph, reminding us that with innovation and perseverance, even the most daunting genetic diseases can be challenged.

0 comments