Why Cancer Immunotherapy Fails – The Protein Panic in T-Cells
Introduction
Cancer immunotherapy has revolutionized oncology, yet many treatments fail due to T-cell exhaustion. On October 3, 2025, Mario Nawfal highlighted a groundbreaking study from Ohio State University Wexner Medical Center revealing the core reason behind this failure: a previously unknown proteotoxic stress response in T-cells (TexPSR). This discovery may transform cancer treatment, offering a method to restore T-cell function and boost therapy effectiveness.
SCIENTISTS UNCOVER WHY CANCER IMMUNOTHERAPY FAILS - AND IT’S A PROTEIN PANIC ATTACK
— Mario Nawfal (@MarioNawfal) October 3, 2025
Turns out cancer-fighting T cells aren’t lazy, they’re just drowning in misfolded protein garbage, thanks to a stress system with the very chill name TexPSR.
Instead of slowing down to recover,… https://t.co/RkdnIDnNE1 pic.twitter.com/zAb1haTYwW
The Discovery Explained
Researchers discovered that T-cells, the immune system’s frontline fighters against cancer, are not inherently ineffective—they are overwhelmed by misfolded protein “garbage” due to TexPSR. Instead of slowing down to manage stress, T-cells accelerate harmful processes, ultimately dying and losing their ability to attack tumors.
Blocking TexPSR in experimental studies allowed T-cells to recover and regain cancer-fighting capabilities, hinting at a potential therapeutic strategy that could dramatically improve immunotherapy outcomes.
BREAST CANCER DRUG SHOWS PROMISE IN MAJOR TRIAL
— Mario Nawfal (@MarioNawfal) September 22, 2025
Roche’s new drug giredestrant, tested with everolimus, helped patients with a serious form of breast cancer live longer without the disease getting worse.
The trial focused on ER-positive, HER2-negative breast cancer - one of the… https://t.co/axrKwawEzb pic.twitter.com/g9OUHaM3iH
Key Insights from the Study
- TexPSR Defined: A stress response in exhausted T-cells causing toxic protein buildup.
- Impact on Immunotherapy: T-cell exhaustion limits cancer treatment effectiveness.
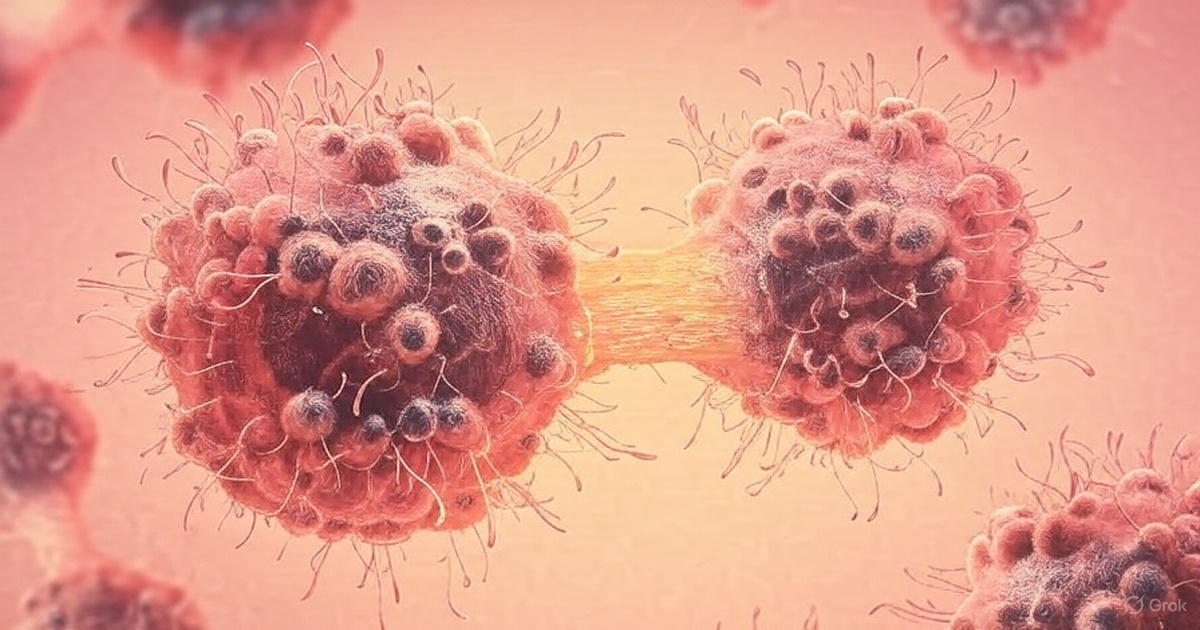
- Visual Evidence: Imaging shows T-cells overwhelmed by misfolded proteins.
- Solution Identified: Blocking TexPSR restores immune function.
- Potential Treatment Implications: Could enhance current immunotherapy protocols.
- Relation to Other Studies: Connects with DNA-based cancer therapies and non-invasive detection technologies.
- Public Engagement: The discovery sparked global discussions and made complex science accessible.
Scientific Context
The discovery emphasizes protein homeostasis—cells managing protein folding and degradation. Misfolded proteins, if unmanaged, can form aggregates toxic to T-cells, similar to mechanisms seen in neurodegenerative diseases. By calming stressed cells rather than attacking tumors aggressively, researchers can potentially enhance immunotherapy effectiveness with fewer side effects.
Broader Impact on Cancer Research
This finding integrates with recent advancements in AI detection tools, DNA-based therapies, and blood flow’s role in tumor growth. It represents a shift from purely external interventions to internal cellular regulation, potentially redefining the future of cancer treatment.
🇬🇧“JUNK” DNA JUST TURNED INTO CANCER’S WORST NIGHTMARE
— Mario Nawfal (@MarioNawfal) September 27, 2025
Scientists in the UK have found a way to kill blood cancer cells by turning their own broken DNA against them.
Turns out, so-called “junk” DNA (the stuff scientists used to ignore) goes haywire in certain cancers, ripping… https://t.co/Q6WxEuCH0u pic.twitter.com/EDMVkO1wgP
FAQs
Q1: What is TexPSR?
TexPSR stands for T-cell proteotoxic stress response, a mechanism that overwhelms T-cells with misfolded proteins.
Q2: How does blocking TexPSR help?
Inhibition of TexPSR restores T-cell function, enabling the immune system to fight cancer effectively.
Q3: Is this applicable to all cancers?
Current studies are preclinical but show promise for multiple cancer types treated with immunotherapy.
Q4: How soon can this lead to new treatments?
Clinical trials and further research are needed; the timeline could range from a few years to a decade.
Q5: Why is this discovery important?
It shifts focus to internal cellular processes, potentially making cancer treatment more effective and less invasive.
Conclusion
The discovery of TexPSR and its role in T-cell exhaustion represents a paradigm shift in immunotherapy research. Rather than solely developing drugs to kill cancer cells, scientists are now focusing on enhancing the body’s internal immune regulation. While challenges remain in translating these findings into widespread clinical practice, the potential impact is enormous. By understanding and controlling cellular stress, immunotherapy could become more effective, safer, and personalized. This insight is a reminder that sometimes, solving complex problems requires listening to the cells themselves, not just attacking the disease.

0 comments